You're moving through your day when you realize something is off. You check the calendar and think: Wait, why is my period early? An early period can happen for all sorts of reasons, from hormonal shifts during perimenopause to recent stress, illness, or travel. Most of the time, it's a normal, temporary change—but sometimes, it's a sign to check in with a healthcare professional.
At Midi, we've seen it all and understand just how unsettling period changes can be. After all, when you reach midlife, you probably thought the days of surprise periods were over. Unfortunately, perimenopause can be a lot like puberty 2.0 with unexpected changes due to hormonal fluctuations that can catch you off guard. Here, we'll cover the most common reasons your period might show up ahead of schedule and the signs it's time to take a pregnancy test or talk with a clinician.
Few things are as annoying as your period showing up when you weren't expecting it. Beyond the inconvenience, you're probably wondering: Why did my period come early, and what can I do about it?
An early period happens when your menstrual cycle is shorter than usual, and bleeding starts days before you expected it. But here's the thing to keep in mind: Your cycle doesn't operate on a fixed schedule. It can shift with things like stress, sleep changes, and travel. Hormone fluctuations during perimenopause and other life stages can affect when you get your period, too.
So an occasional early period doesn't necessarily mean something is wrong. Here, we’ll break down how to recognize an early period, what typically triggers it, when early bleeding might require medical attention, and practical ways to track your cycle.
What Counts as an Early Period?
Before we dive into why your period showed up early, let’s define an early period. An early period means your cycle is shorter than usual, so your period comes sooner than expected.
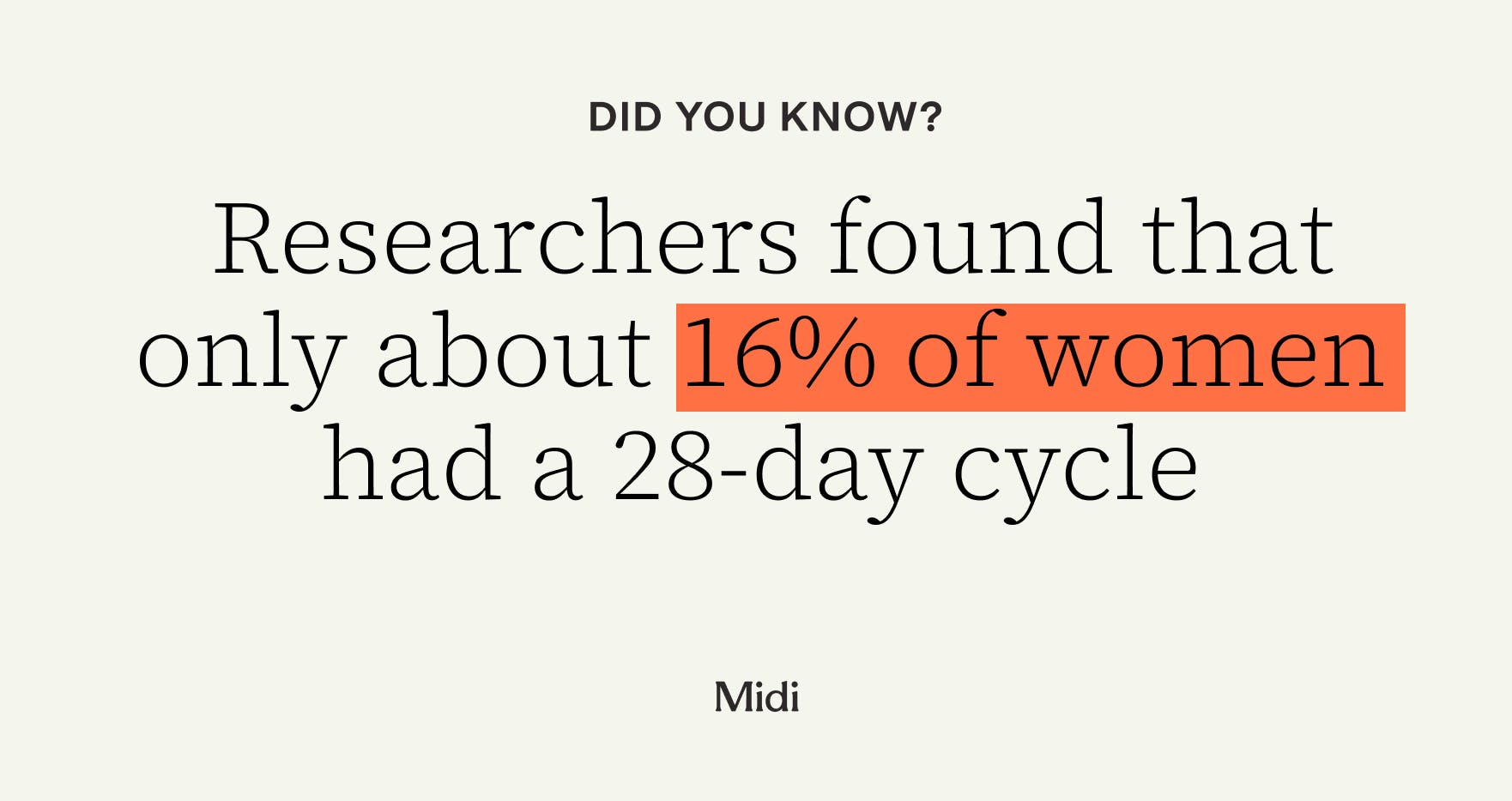
Typically, a “normal” menstrual cycle lasts about 24 to 38 days, with 28 days being the average. But everyone’s cycle is different. In a study of more than 1 million women, researchers found that only about 16% had a 28-day cycle. So an early period is about changes to your personal baseline.
Sometimes, unexpected or mid-cycle bleeding isn’t a period at all. Understanding the differences can put you one step closer to figuring out what’s going on:
- A true period: This marks the start of a new cycle. It typically shows up with your usual flow and symptoms.
- Breakthrough bleeding: Also known as spotting, it occurs between your usual periods and is usually lighter than your typical flow. It’s a common side effect of hormonal birth control and can happen with other hormonal shifts like perimenopause.
- Withdrawal bleeding: This happens when hormones drop during the placebo week of hormonal birth control.
- Implantation bleeding: This refers to bleeding or spotting that may happen in early pregnancy. It starts around the time you expect your period, but it’s usually much lighter and shorter.
Is It Normal for My Period to Come Early?
Yes, an early period, no matter how frustrating, can be completely normal.
“A lot of people don’t understand that their period really is part of a cycle,” says Midi Health clinician Sonya Carothers, APRN, PhD, FNP. “It happens every so many days, not necessarily on the exact same calendar day every month.”
The occasional early or late period is not usually a red flag. It may be tied to lifestyle changes like high stress or travel, and in most cases, your cycle settles back into its usual rhythm the next month. Changes matter more when they become part of a pattern, usually over two to three cycles. It doesn’t mean anything is wrong, but it can help you identify triggers that affect your cycle.
Common Short-Term Triggers
Many factors in your daily life, from your sleep habits to your exercise routine, can make your period come early. It’s annoying, especially if you’re used to your cycle running like clockwork, but it’s not usually a cause for concern.
Acute stress
Stress can take a toll on your mental and physical health, including your menstrual cycle. When you’re under pressure, your body releases more cortisol, a stress hormone that can disrupt estrogen and other hormones, like cortisol, that regulate the menstrual cycle. That disruption can lead to cycle changes like an early period or differences in flow.
Poor sleep
Changes to your sleep schedule––whether from poor or inadequate sleep, travel across time zones and jet lag, or shift work––disrupt your circadian rhythm. This internal clock controls your sleep-wake cycle and helps regulate hormones. So when that rhythm is thrown off, it can contribute to menstrual cycle changes, including when your period shows up and how heavy or light it is.
Recent illness
Even a mild illness, like a cold or flu, can temporarily affect cycle timing. Hormones may shift as your body prioritizes fighting off the viral infection. Many people may notice menstrual cycle changes, like an early period, in the first few months after being sick.

Intense exercise or weight changes
Rapid weight changes or sudden changes in exercise intensity—especially when you’re not eating enough––can stress your body and interfere with hormone levels. This physical stress may trigger an early period or change your flow.
Birth control and medication changes
Your birth control and certain medications can also affect when your period shows up. You might notice temporary changes, such as an early period or different flow.
Starting, stopping, or missing hormonal contraception
When you start a new hormonal birth control method like the pill, patch, or ring, your body needs time to adjust. Breakthrough bleeding, lighter or shorter periods, or a period that comes earlier or later than expected is common in the first few months. Similarly, when you stop hormonal contraception, early bleeding or spotting may occur as hormone levels shift. Missing pills or forgetting to change the patch or ring can also trigger early or unexpected bleeding as hormone levels drop.
IUD changes
Perhaps unsurprisingly, IUDs can also affect your menstrual cycle. Hormonal IUDs may cause irregular or unpredictable bleeding in the first 3 to 6 months after insertion. Copper IUDs don’t have any hormones, but they may initially cause heavier or longer periods and more cramping.
Emergency contraception
Emergency contraception like Plan B or ulipristal contains hormones that delay or prevent ovulation, which can cause spotting or make your next period come earlier or later than usual. But your period should return to normal––whatever that looks like for you––after one cycle.
Other medications
Several other medications can also affect period timing or flow. Blood thinners (anticoagulants), for example, might not make your period come early, but they can cause heavier, longer, or irregular bleeding. This is because they affect how your blood clots. Some antidepressants and antipsychotics have been linked to irregular cycles and heavier bleeding. Corticosteroids like prednisone can also temporarily affect your cycle.
Life stage factors
Estrogen, progesterone, and other hormones naturally change as you age, so your cycles might be different at various stages of life. When you first started your period, your cycles may have been all over the place––think heavy, early, late, or missing altogether. But with time, your periods probably became more predictable as hormones matured and ovulation became more consistent.
Still, your hormones shift at other key points in life. If you are postpartum or breastfeeding, irregular, early, or late periods are common as your cycle resets to pre-pregnancy levels.
You might feel like a teenager again by the time you reach perimenopause, which usually starts in your mid 40s, but can begin as early as your late 30s or as late as your 50s. During this transition phase leading up to menopause, estrogen and progesterone levels fluctuate, making your periods unpredictable. In fact, an irregular period is often one of the first signs of perimenopause for many women.
Depending on which stage of perimenopause you’re in, you might have:
- shorter or longer cycles
- missed periods
- spotting between periods
- heavier or lighter flow
- shorter or longer bleeding days
Medical Conditions That Can Cause an Early Period and Cycle Changes
An early period is often harmless and usually the result of natural hormonal changes and short-term triggers. (Same thing with a late one, too!) But sometimes it can be a sign of certain medical conditions, especially when accompanied by symptoms such as pain, dizziness, or fatigue:
- Thyroid disorders: The thyroid is a small gland in the neck that helps regulate your menstrual cycle. Thyroid disorders, such as hypothyroidism and hyperthyroidism, have been linked to irregular periods.
- Hyperprolactinemia: Breastfeeding and certain medications may cause this condition, which can interfere with ovulation and lead to irregular or missed periods.
- Polycystic ovary syndrome (PCOS): Long or inconsistent cycles are a common symptom of PCOS, so bleeding may show up earlier or later than you expect.
- Fibroids or polyps: These benign growths in or on the uterus may cause heavier or longer bleeding and spotting that might feel like an early period.
- Endometriosis or adenomyosis: With endometriosis, tissue grows outside the uterus, and with adenomyosis, tissue grows inside the uterine wall. Both have been linked to painful periods, heavy bleeding, and spotting.
- STIs or pelvic infections: Conditions like chlamydia or pelvic inflammatory disease can cause unexpected bleeding that feels like an early period. You should see a healthcare professional if you also have pelvic pain, unusual discharge, or fever.
- Early miscarriage: Early pregnancy loss can look like an early or heavy period. If you have heavier bleeding or cramping, or if you pass tissue, it’s important to take a pregnancy test and seek medical care.
- Iron deficiency: Heavy or frequent bleeding can lead to low iron. Watch for common symptoms like fatigue and dizziness.
Could an Early Period Mean I’m Pregnant?
Yes, sometimes what looks like an early period is actually implantation bleeding, one of the earliest signs of pregnancy. Implantation bleeding occurs when a fertilized egg attaches to the uterine lining. It usually happens around 6-10 days after ovulation or conception or just before you expect your next period, so it’s easy to confuse the two.
But there are some key differences. Implantation bleeding tends to be lighter and shorter than a true period and it can last hours to up to three days after implantation. You might have pink or brown spotting or a light flow that isn’t heavy enough to fill a pad or tampon for anywhere from a few hours to a few days. An early period usually has a clearer start, starts heavier, and lasts for at least a couple of days.
Take a pregnancy test if you had sex during your fertile window, the bleeding is lighter or shorter than usual, and you notice other early pregnancy symptoms like breast tenderness or nausea. If the first test is negative but bleeding continues and symptoms remain unclear, take another test in 48 to 72 hours. Pregnancy hormones increase quickly in early pregnancy, so a second test may be positive.

What to Do if Your Period Comes Early
Try not to worry if your period comes early. Instead, focus on these simple steps to find out what’s happening and how to get your cycle back on track.
Track your cycle
Try a journal, app, or wearable tracker to log when bleeding starts and stops, your flow, pain or cramps, and possible triggers like stress, travel, or missed pills. Tracking two cycles can tell you whether an early period is a one-off or a pattern.
Revisit your routine
Some lifestyle tweaks can help your cycle bounce back. For example:
- Prioritize sleep: Aim for 7 to 9 hours per night, and try to go to bed and wake up at the same time every day, if you can. Consistent, restful sleep helps keep your hormones balanced.
- Eat balanced, protein-rich meals: Nutrient-dense meals provide steady energy and help keep your hormones stable throughout the day.
- Ease up on intense training: If you’ve been overdoing it or not recovering properly, scale back for a week. Too much physical stress can make your cycle wonky.
- Manage stress where you can. “Stress can make cycles come earlier or later,” says Dr. Carothers, “so anything that truly lowers stress can help.” She says it’s less about balancing your hormones and more about giving your whole body a reset. Simple ways to lower stress—like walking, taking a hot bath, or doing some deep breathing—can help make life feel more manageable.
Take a pregnancy test
If there’s any chance you might be pregnant, take a test. Repeat the test in 48 to 72 hours if you’re still not sure about your symptoms.
Check your birth control
If you missed pills or doses or recently switched methods, follow the catch-up instructions on your hormonal birth control package and use backup contraception as directed.
Working With a Healthcare Professional
Loop in a healthcare professional, like a Midi clinician, if your period comes early a few cycles in a row, it’s unusually heavy or painful, or you just have questions. A little prep can help you get the most out of your visit.
Bring the basics to your appointment, including:
- 2 to 3 months of cycle logs and symptoms
- a list of your current medications and supplements
- details about any recent emergency contraception use
From there, your clinician can decide which evaluations make sense for your situation. They might start with a pregnancy test, basic labs like a CBC and ferritin to check for low iron or anemia, or hormone tests such as TSH to assess thyroid function or prolactin if your cycles are irregular. Depending on your symptoms, they may also recommend STI screening, a pelvic exam, or an ultrasound.
And don’t be shy about asking all the questions, even ones that can feel embarrassing or stuff you feel like you “should know by now.”
You can work with your healthcare professional to create a plan that works for you. It might include addressing lifestyle triggers, adjusting your birth control method, or treating any underlying conditions. Your clinician will also set a clear timeline for how many cycles to track and when to follow up.
When to Seek Immediate Care
A one-off early period isn’t usually a problem, but some symptoms require immediate medical attention. If you've had a regular cycle and then start bleeding again within a week or two without starting birth control or hormones—or if bleeding lasts longer than about 10 days—it’s important to be evaluated in person, says Dr. Carothers. Even virtual care clinics, like Midi, can refer you for in-person testing if necessary.
You should also see a healthcare professional right away if you have any of these symptoms:
- Soaking through one of more pads or tampons within 1-2 hours more than once in a day.
- large blood clots, severe dizziness, or fainting
- a positive pregnancy test with heavy bleeding or one-sided pain
- bleeding after sex or between periods for more than two cycles
- new period changes if you’re under age 9, over age 55, or postmenopausal
Key Takeaways
- If you’re asking “why is my period early,” a one-off change is usually normal. Stress, travel, poor sleep, illness, or routine disruptions can temporarily shorten your cycle.
- Hormonal shifts often explain early periods. Changes in estrogen and progesterone, especially during perimenopause, postpartum, or after starting or stopping birth control, can cause bleeding to start sooner than expected.
- Not all early bleeding is a true period. Spotting, breakthrough bleeding, withdrawal bleeding, or implantation bleeding can mimic an early period but usually look lighter or shorter.
- Certain medical conditions can trigger early or irregular cycles. Thyroid disorders, PCOS, fibroids, infections, or early pregnancy loss may cause bleeding that feels like an early period.
- Tracking patterns helps determine next steps. Logging cycle length, flow, symptoms, stress, and medication changes can clarify why your period is early and when to seek medical care.
Frequently Asked Questions (FAQs)
What causes early periods?
Early periods can happen when your hormones shift––from stress, travel, or even changes to your sleep routine. Perimenopause, starting or switching birth control, and certain medications also trigger hormonal changes that may affect when your period shows up. Usually, your cycle returns to its typical pattern the next month.
Is it normal for your period to come 2 weeks early?
A one-off early period can be normal, especially if you’ve recently been stressed or sick, or if you started a new medication. Cycles can change from month to month, so it’s not unusual for period timing to be off once in a while. But if early periods become a pattern over two to three cycles, or you notice heavier bleeding or other new symptoms, it’s worth checking in with a healthcare professional.
Can an early period mean I’m pregnant?
Technically, yes. Sometimes, early bleeding that looks like an early period is actually implantation bleeding, a very early sign of pregnancy. Implantation bleeding is usually a lot lighter and shorter than a true period. Take a test if there’s any chance you might be pregnant.
Can stress cause my period to come early?
Yes, stress is one of the biggest lifestyle factors that can change your cycle, says Dr. Carothers. When you’re stressed, your hormones fluctuate in ways that can throw off your cycle, making your period come earlier or later than usual. Simple habits like taking a few minutes to stretch or move your body throughout the day can help you keep stress in check.
If you’re in perimenopause or menopause and want guidance from clinicians who specialize in women’s midlife health, book a virtual visit with Midi today.
Hormonal change is at the root of dozens of symptoms women experience in the years before and after their period stops.
Our trained menopause specialists can help you connect the dots to guide you towards safe, effective solutions.
Whether you need personalized guidance or a prescription routine to tackle symptoms—including brain fog, hot flashes, sleep trouble, mood swings, and weight gain—we’ve got you covered. Learn more here.
Midi’s mission is to revolutionize healthcare for women at midlife, wherever they live and whatever their health story. We believe that starts with education, to help all of us understand our always-changing bodies and health needs. Our core values guide everything we do, including standards that ensure the quality and trustworthiness of our content and editorial processes. We’re committed to providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. For more details on our editorial process, see here.