Roughly 6,000 women in the United States are welcomed into the menopause club every single day. Menopause brings some serious hormonal shake-ups that can trigger life-changing symptoms in the run-up to your final period and linger long after. But here's the good news: With smart treatments like hormone replacement therapy (HRT), botanicals, supplements, and some lifestyle tweaks, those hot flashes, mood roller-coasters, and bedroom blues can totally be tamed. Think of this as your menopause survival guide—we've got you covered.
What is menopause? This is honestly one of the biggest plot twists in a woman's life—and spoiler alert: Every single one of us will experience it if we live long enough. Sure, you might deal with some pretty intense symptoms for a few years, but here’s plot twist number two: This phase can actually be pretty amazing. The secret sauce? Getting the right menopause treatment can completely transform how you feel during this wild ride.
Let's dive into what's actually happening during menopause, when this party starts, the symptoms that might crash your daily routine, the best treatments that actually work, the lifestyle changes that are total game-changers, and how to build your support squad. We've totally got your back on this journey.
Stages of Menopause
Menopause isn't just one event—it's like a three-act play that unfolds in midlife and beyond. Here's the breakdown:
Perimenopause
Perimenopause is the opening act—the phase leading up to menopause, when your hormones decide to go completely rogue. Estrogen and progesterone start their gradual decline, but they're not going quietly. Instead, they're bouncing around like ping-pong balls, and all that hormonal chaos triggers the classic perimenopause symptoms: irregular periods that show up whenever they feel like it, hot flashes that make you feel like you're spontaneously combusting, night sweats that turn your bed into a swamp, mood shifts worthy of an Oscar, sleep that becomes more elusive than a unicorn, and libido and arousal changes that nobody warned you about.
So, when does menopause start? Perimenopause typically crashes the party in your mid-40s, but some lucky ladies get an early invitation in their 30s, while others don't get the memo until their 50s. And how long does menopause last? Most women ride the perimenopause wave for about 4 years, but some get the extended director's cut that can last up to 10 years. Unfortunately, there's no crystal ball to tell you exactly how long your personal perimenopause adventure will be.
Menopause
This is the climactic moment—menopause officially marks the end of your baby-making years. We might say we're "going through menopause," but menopause is actually more like a single day on the calendar. Once you've gone 12 consecutive months without a period (and yes, we're counting every single day), you've officially crossed the menopause finish line. The average menopause age for this milestone is 51, but like everything else in this journey, we're all beautifully different—some hit this mark years earlier, and others reach it years later.
Postmenopause
This is basically the rest of your life. But, even after you’ve waved goodbye to periods once and for all, that doesn’t mean all your symptoms go away. For some, symptoms may dissipate. For others, they can keep raging on.
Signs and Symptoms of Menopause
Hormonal ups and downs in menopause trigger symptoms from head to toe that can affect your physical and mental well-being. Considering the list below, it’s no surprise that women who experience more menopause symptoms report a worse quality of life, according to research. Not every woman experiences all of these symptoms, though—and some don’t have any symptoms at all.
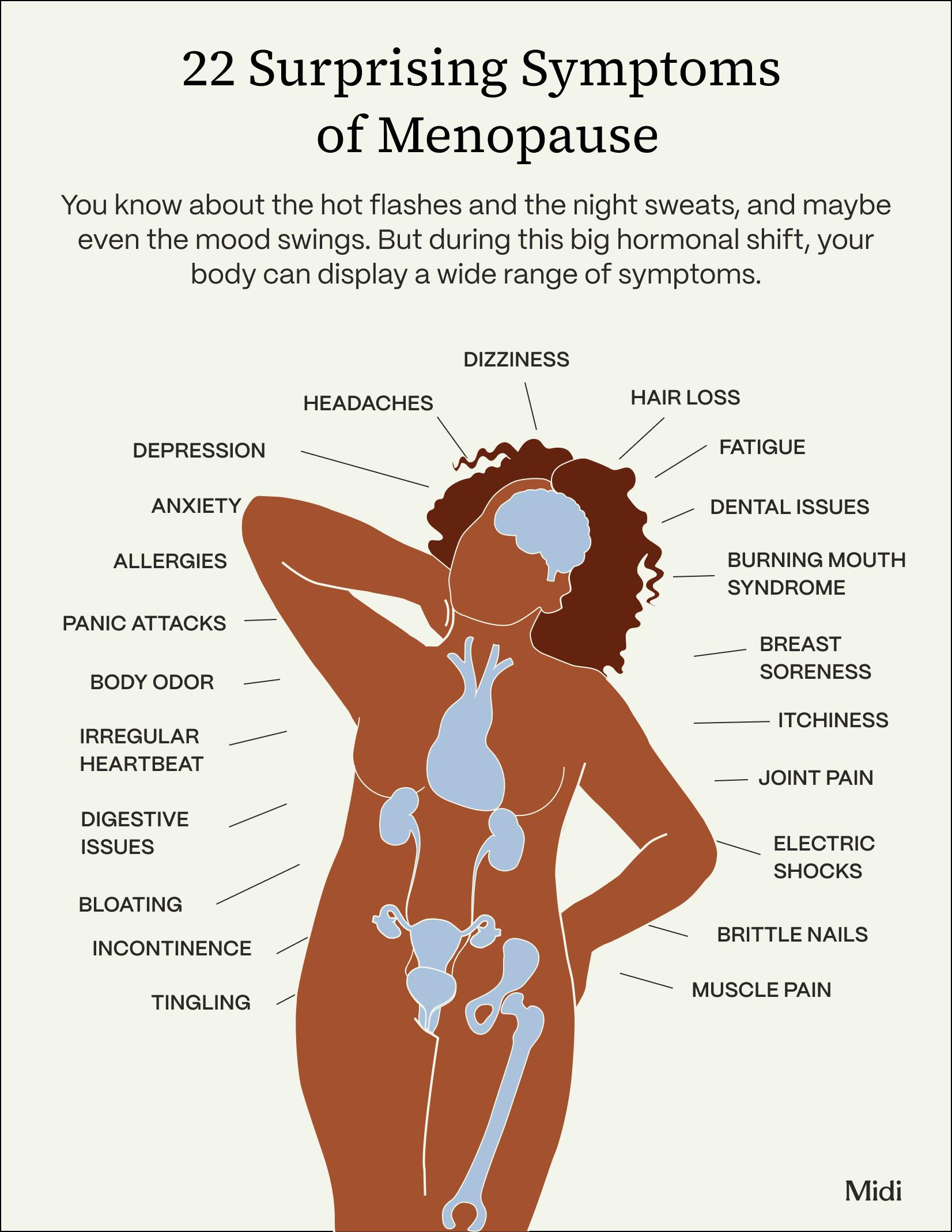
Here’s a brief look at some of the most common signs of menopause:
Physical symptoms
Some physical symptoms of menopause are more expected than others. But with this list of possibilities, it’s fair to say be prepared for anything:
- hot flashes
- night sweats
- urinary incontinence
- vaginal dryness
- fatigue
- breast changes
- joint pain
- acne
- itchy skin
- heart palpitations
- weight changes
- irregular periods
Emotional and cognitive symptoms
Hormonal changes, midlife stress and responsibilities, and the physical symptoms of menopause can affect your mood and memory, causing symptoms like:
- anger
- anxiety
- brain fog
- depression
- forgetfulness
- irritability
- mood swings
- panic attacks
- social withdrawal
Sexual health changes
One in seven women say that sexual health symptoms cause significant distress in midlife. These include:
- decreased libido
- pain or discomfort during intercourse
- vaginal dryness
Health Risks and Complications
Estrogen is healthy for your body’s tissues, including for your heart, bones, urinary system, and more. With lower levels of estrogen and progesterone, you may be at an increased risk of:
- Osteoporosis and bone density loss: Estrogen loss speeds up the loss of bone mass, which leaves your skeleton weaker and more vulnerable to fracture.
- Cardiovascular risks: A lack of estrogen after menopause increases the risk of cholesterol buildup in the arteries, raising the risk of heart disease and stroke in women.
- Urinary incontinence and bladder issues: You may have trouble with leakage or urgency.
- Weight management challenges: Of Midi patients, 87% say they’ve experienced weight gain and body changes. Estrogen depletion triggers muscle loss and causes an increase in body fat, especially abdominal fat. Lifestyle changes, such as being more sedentary, lack of sleep, or increased stress, can also set the stage for weight gain.
- Increased risk of certain cancers: Menopause itself does not increase your risk of cancer, but aging does. You have an increased risk of breast, endometrial (uterine), cervical, and colorectal cancers, among others.
Menopause Diagnosis and Medical Evaluation
Think you've joined the perimenopause club? Time for a talk with a healthcare professional you trust. You should have a thorough chat about your health history and symptoms—basically, they need to figure out if your body's recent weirdness is due to hormonal changes or something else entirely.
At Midi Health, we're team players with The Menopause Society and don't usually recommend routine hormone testing for most women to determine whether you’re in perimenopause. Here's why: Your hormone levels are basically doing the wave all day long, so a single test is about as useful as a weather forecast from last month. That said, hormone testing might be helpful in certain situations—like figuring out the perfect treatment combo to kick your symptoms to the curb.
Treatment Options for Menopause Symptoms
Here's the beautiful truth: Even though menopause can throw some seriously debilitating symptoms your way, we've got an impressive list of strategies to help you fight back. The best approach usually involves mixing and matching hormonal treatments, nonhormonal options, natural remedies, and lifestyle changes. Think of it as creating your personalized menopause battle plan.
A thorough conversation with a menopause-savvy clinician will help you build a care plan that fits your specific needs and preferences. Treatment options might include:
Hormone Replacement Therapy (HRT)
Also called hormonal therapy or menopausal hormone therapy, HRT is like sending in reinforcements—it gives your body just enough estrogen to tell symptoms like hot flashes, night sweats, vaginal dryness, irregular periods, and mood shifts to take a hike. If you still have your uterus, you'll also get progesterone. That’s because estrogen can thicken the uterine lining—and that’s a known risk factor for uterine cancer. Taking progesterone while taking estrogen is key because it reduces this thickening and brings the uterine cancer risk back to baseline.
HRT can work for most women, but that doesn't mean it's right for every woman. After a comprehensive exam and deep dive into your health history, a menopause specialist can tell you whether HRT should be in your game plan.

Non-hormonal Medical Treatments
Women who want to avoid hormonal treatment still have a variety of nonhormonal options, including:
- Local vaginal estrogen, which stays put and doesn't travel through your whole system and can tackle those uncomfortable genitourinary symptoms
- Certain antidepressants that can treat hot flashes and mood symptoms.
- Veozah, a non-hormonal, oral prescription medication that’s effective at treating moderate to severe hot flashes and night sweats
- Weight loss medications, such as GLP-1 agonists like semaglutide, may be prescribed as an addition to a healthy lifestyle.
True Stories Of Transformation
Natural and Alternative Treatments
A healthcare professional might recommend certain herbal supplements and alternative treatments in lieu of or alongside hormone therapy. For example, botanicals such as black cohosh is a well-studied treatment for hot flashes for some women. Cognitive behavioral therapy can also play a role in menopause management.
Lifestyle Changes to Manage Menopause Symptoms
What you eat, how you move, and how you handle stress can seriously impact how often and how intensely menopause symptoms show up. Here's your action plan:
Diet and nutrition
Although there is no one “menopause diet” for everyone, experts recommend a healthy, balanced eating plan. A decrease in estrogen during menopause reduces your body’s calorie burn by 250 to 350 calories per day. Following a plant-based diet that includes plenty of lean protein—think vegetables, fruit, low-fat dairy, whole grains, legumes, fish and seafood, poultry, eggs—can help keep you satiated and preserve muscle, both of which are cornerstones of weight management.
Exercise and physical activity
Exercise isn't just about burning calories (though that's nice, too). It builds and maintains muscle and bone, strengthens your heart, regulates your mood, improves your sleep, and kicks stress to the curb. Women should aim for a triple threat: aerobic exercise, strength training, and flexibility work. Your body will thank you in about a million different ways.
Stress management
Let's be real: Hot flashes are stressful. Waking up at 3 a.m. drenched in sweat and unable to fall back asleep? Also stressful. And midlife in general? Ridiculously stressful.
Good stress management protects your mental health, keeps brain fog at bay, and helps you make choices that actually support your well-being. The key is finding techniques that resonate with you. Your options include cognitive behavioral therapy (CBT), meditation, mindfulness, yoga, stretching, progressive muscle relaxation, exercise, deep breathing, time in nature, and walking. Pick your favorites and make them nonnegotiable parts of your routine.
Mental and Emotional Well-Being During Menopause
Okay, let's talk about what's really going on during midlife. Even if you didn't have to deal with hormonal chaos right now, it would still be totally understandable if your memory was acting like a broken GPS, your mood was more volatile than cryptocurrency, and anxiety was your uninvited constant companion.
A full 70% of menopausal women deal with mood shifts. Estrogen plays a starring role in neurotransmitter function (those brain chemicals that keep your mood stable), so when estrogen takes a dive, your emotional equilibrium can go with it. Add in career pressures, caring for kids AND aging parents, financial stress, relationship changes, and all the other midlife plot twists, and it's honestly amazing any of us are functioning at all.
Your coping strategy toolkit can include lifestyle changes (regular exercise is seriously underrated for mental health), CBT, botanical supplements, prescription medications, HRT, or a combination of all the above. Depression and anxiety during menopause are totally treatable—you don't have to white-knuckle your way through this.
Sexual Health and Intimacy
Vaginal dryness, discomfort, pain, reduced arousal, disappearing libido—these issues are like unwelcome party crashers during menopause, all thanks to estrogen taking an extended vacation. But here's what you need to know: Menopause's effects on your sex life are highly treatable. You absolutely do not have to accept "Well, this is just how it is now" as your final answer.
Maintaining a healthy sex life during these years has real benefits: deeper intimacy in relationships, stress relief, and improvements in self-esteem. Plus, let's be honest—you deserve to feel good in your own skin and enjoy physical pleasure.
Your treatment options are plentiful, including HRT, vaginal moisturizers and lubricants, vaginal estrogen, sex therapy, medications and vibrators to enhance arousal, pelvic floor physical therapy, testosterone, and lifestyle adjustments like regular exercise (it really does help with everything). A consultation with a healthcare professional, like a Midi clinician, can help you find the perfect combination to get your groove back.
Menopause in Special Circumstances
Not everyone gets the "typical" menopause experience around age 51. Sometimes, life throws curveballs:
- Early or premature menopause: Premature menopause is menopause that occurs before age 40, affecting 1% of U.S. women. Early menopause is menopause between ages 40 and 45, which affects about 5% of U.S. women. Risk factors for early or premature menopause are smoking, chemotherapy and radiation during cancer treatment, family history, chronic stress (such as PTSD), and certain diseases like autoimmune-related thyroid disease.
- Surgical menopause: When both ovaries are removed surgically, you get instant menopause—no gradual transition, just boom, welcome to the club. Before having this surgery, make sure you have a thorough conversation (probably multiple conversations!) about what this means for your health and how to manage sudden, dramatic hormonal changes. HRT often becomes a cornerstone treatment for women experiencing surgical menopause.
Preventive Health and Long-Term Care
Menopause's hormonal changes affect your body so profoundly that your previous barely-any-doctor-visits approach needs a major upgrade. Regular health screenings are now critical for checking on your current health and assessing future risks. Catching issues early gives you the best shot at treating them before they become bigger concerns.
Your action plan: Stay up-to-date with vaccinations and preventive screenings, keep those routine health visits with a healthcare professional you trust, and when you notice changes in your health—especially anything that concerns you—make that appointment and actually show up for it. Your future self will be so grateful.
Common Myths and Misconceptions About Menopause
Menopause has been stigmatized for way too long, which is honestly ridiculous since literally every woman will experience it. Thanks to that stigma (and some seriously misplaced shame), we need to set the record straight on a few major myths:
- Suffering due to menopause symptoms is inevitable: Absolutely not! We have an amazing range of effective treatments that can help you feel like yourself again. You don't have to grin and bear it.
- You can balance your hormones: That’s pseudoscience— hormone levels change from hour to hour. No magic supplement can create perfect hormonal harmony. That said, declining estrogen definitely triggers menopause symptoms, so potentially supplementing with estrogen through HRT can seriously reduce their impact.
- HRT is not safe: This myth comes from 20-year-old data that's been misunderstood and misrepresented. Recent research actually shows that HRT decreases the risk of heart disease and bone loss when prescribed appropriately. For many women, HRT can be a safe, effective option throughout the menopausal transition.
Resources and Support
At Midi, we're all about amplifying the conversation surrounding menopause. Every day, 6,000 women (you read that right!) officially hit menopause in the United States.
Here’s where to find extra support:
- menopause podcasts
- menopause support groups and other resources in your community
- patient and education resources from The Menopause Society
- books like Hot and Bothered and Estrogen Matters
- menopause support and other resources on JoinMidi.com
Key Takeaways
- We consider menopause to have three stages: perimenopause (the years before menopause), menopause (when periods have stopped for 12 consecutive months), and postmenopause (after menopause for the rest of your life).
- Menopause symptoms are far-reaching and extremely impactful on a woman’s well-being, causing physical distress; mental, emotional, and cognitive changes; and sexual health and intimacy issues, among others.
- Various options for treatment exist—and they work. Working with a clinician to draw up an individualized care plan is your best chance at finding relief, which may include hormonal therapy, nonhormonal medical treatments, botanicals and supplements, and lifestyle changes.
- Support during menopause can help you thrive during this new stage of midlife. Resources like books, podcasts, support groups can help as can finding a trained menopause specialist, like via Midi Health.
Frequently Asked Questions (FAQs)
How does menopause affect daily life?
Menopause can seriously shake up your daily routine with sleep disruptions, surprise hot flashes, mood roller-coasters, brain fog that makes you forget why you walked into a room, and vaginal dryness that affects intimacy. Together, these symptoms can make you feel like a stranger in your own body. The important thing to remember? Don't brush them off, because safe, effective treatments can help you feel like yourself again.
What does menopause do to a woman?
During the menopause transition, your estrogen and progesterone levels go on a wild roller-coaster ride, triggering all those fun symptoms we've been discussing. As you move through perimenopause, these hormones gradually decline until they hit rock bottom, officially ending your fertile years. Once you've gone 12 consecutive months without a period, you've completed the menopause journey.
Can menopause cause depression?
Absolutely. Women are up to three times more likely to experience depression during the menopausal transition compared to premenopause. When estrogen levels drop, it affects neurotransmitters—those brain chemicals responsible for keeping your mood stable. What you’re feeling is valid and treatable..
What to do when menopause starts?
When menopause symptoms start crashing your party—from the obvious ones like hot flashes and vaginal dryness to the sneaky ones like tooth sensitivity, joint pain, and heart palpitations—connect with a clinician who actually specializes in menopause, like a Midi Health clinician. Together, you can develop a personalized plan that addresses your specific symptoms, fits your lifestyle, and matches your treatment preferences, so you can feel amazing again.
If you’re in perimenopause or menopause and want guidance from clinicians who specialize in women’s midlife health, book a virtual visit with Midi today.
Hormonal change is at the root of dozens of symptoms women experience in the years before and after their period stops.
Our trained menopause specialists can help you connect the dots to guide you towards safe, effective solutions.
Whether you need personalized guidance or a prescription routine to tackle symptoms—including brain fog, hot flashes, sleep trouble, mood swings, and weight gain—we’ve got you covered. Learn more here.
Midi’s mission is to revolutionize healthcare for women at midlife, wherever they live and whatever their health story. We believe that starts with education, to help all of us understand our always-changing bodies and health needs. Our core values guide everything we do, including standards that ensure the quality and trustworthiness of our content and editorial processes. We’re committed to providing information that is up-to-date, accurate, and relies on evidence-based research and peer-reviewed journals. For more details on our editorial process, see here.