MEET MIDI
Expert, Personalized Virtual Care
One-size-fits-all doesn't work for midlife care. Discover science-backed treatments tailored to your specific concerns.
Join more than 230,000 women who love and trust Midi for their midlife care.

REAL WOMEN. REAL RESULTS.
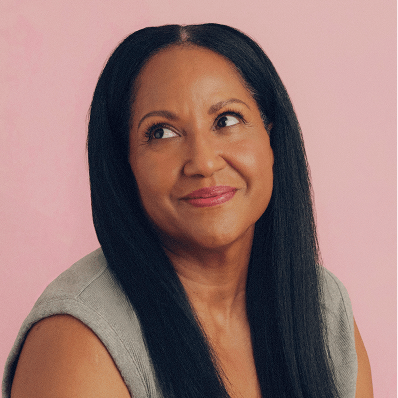
We See You. We Hear You. We Can Help.
Our clinicians specialize in women’s midlife health, so you’ll feel heard from your very first visit. We’re here to help you understand the root cause of your symptoms—and most importantly, offer solutions so you feel relief, asap.
DON’T JUST TAKE OUR WORD FOR IT